CATARACT
A Cataract is a clouding of the lens of the eye. The lens
is a clear oval structure with three layers: the Nucleus,
the Cortex, and the Capsule. It may help to think of the
lens structure as a peach, where the Nucleus is the
peach pit, the Cortex is the flesh of the peach that
surrounds the pit, and the Capsule is the peach skin, or
elastic covering of the lens. You have a Cataract when
the nucleus becomes opaque (that is, it is no longer
clear) or when small opacities develop in the Cortex
that block or scatter light. There are three types of
Cataracts that affect different parts of the lens, have
different symptoms and cause different vision
problems:
Nuclear Cataract is the most common type of
Cataract, and is due to the aging process. The nuclear
gradually hardens and becomes opaque, causing
difficulty identifying colors and seeing at a distance.
Cortical Cataract is the next common type, often
affecting people who are diabetic. Web-shape opacities
develop in the cortex, interfering with passage of light.
This can result in problems with glare and loss of
contrast, as well as difficulty with distance and near
vision.
Sub Capsular Cataract develops under the back
of the capsule or elastic covering of the lens and is
common in people with significant Myopia, Diabetics
who have high Myopia, adults with Retinitis
Pigmentosa, and in people taking Cortisone medication.
This type of cataract can cause glare sensitivity and
blur. In the early stages, only a doctor can detect a
cataract because there may not be any symptoms.
When you do start to notice changes in your vision,
they may include: Blurry distance vision, especially
outdoors, streaks or rays of light seeming to come from
headlights and stop signs. Instinctively shading your
eyes from the sun or feeling more comfortable wearing
a visor. Print appearing faded and lacking in contrast.
Colors appearing faded or changed in hue. Blue may
appear to be green and yellow may look white.
Because these may also be symptoms of other eye
conditions, it is important to see your eye doctor
annually, or when you notice a persistent change in
vision. Cataracts are treated with surgery. Cataract
surgery is an outpatient procedure performed by an
Ophthalmologist. Surgery can often be postponed until
the cataract begins to seriously affect our ability to
function. There is no medicine or treatment that can
dissolve or remove cataracts.
DIABETIC RETINOPATHY
Diabetic Retinopathy is an eye disease caused by
complications of Diabetes. Diabetes causes damage to
the blood vessels that nourish the retina, the seeing
part at the back of the eye.
In people with Diabetes, the retinal blood vessels may
expand and leak fluid. Abnormal new blood vessels
may grow, and blood vessels may break and cause bleeding. These changes may result in vision loss or
blindness. Every person with Diabetes is at risk of
developing Diabetes Retinopathy. The longer a person
has Diabetes the more likely the person is to develop
Diabetic Retinopathy. Regular eye exams are essential
when first diagnosed with Diabetes, and then at least
every two years will reduce your risk of vision loss and
blindness. Vision may not change until the disease is
advanced. Vision loss due to Diabetic Retinopathy can
be prevented if detected and treated early. Tight
control of your Diabetes will delay the development of
Retinopathy.
GLAUCOMA
Glaucoma is a group of eye diseases that gradually
steals sight without warning and often without
symptoms. Vision loss is caused by damage to the optic
nerve. The nerve acts like an electric cable with over a
million wires and is responsible for carrying the images
we see to the brain. The two main types of Glaucoma
are Open Angle Glaucoma and Angle Closure Glaucoma.
Primary Open Angle Glaucoma
This is the most common form of Glaucoma, affecting
about three million Americans. It happens when the
eye’s drainage canals becomes clogged over time. The
inner eye pressure (also called Intra Ocular Pressure
(IOP) raises because the correct amount of fluid can’t
drain out of the eye. With Open Angle Glaucoma, the
entrances to the drainage canals are clear and should
be working correctly. The clogging problem occurs inside the drainage canals, like the clogging that is
inside a pipe below the drain in a sink. Most people
have no symptoms and no early warning signs. If Open
Angle Glaucoma is not diagnosed and treated, it can
cause a gradual loss of vision. This type of Glaucoma
develops slowly and sometimes without noticeable
sight loss for many years. It usually responds well to
medication, especially if caught early and treated.
Angle-Closure Glaucoma
This type of glaucoma is also known as acute glaucoma
or narrow angle glaucoma. It is much rarer and is very
different from open-angle glaucoma in that the eye
pressure usually rises very quickly. This happens when
the drainage canals get blocked or covered over, like a
sink with something covering the drain.
With angle-closure glaucoma, the iris is not as wide
and open as it should be. The outer edge of the iris
bunches up over the drainage canals, when the pupil
enlarges too much or too quickly. This can happen
when entering a dark room.
A simple test can be used to see if your angle is normal
and wide or abnormal and narrow. Symptoms of angle-
closure glaucoma may include headaches, eye pain,
nausea, rainbows around lights at night, and very
blurred vision.
Secondary Glaucoma
Glaucoma can occur as the result of an eye injury,
inflammation, tumor, and in advanced cases of Cataract
or Diabetes. It can also be caused by certain drugs,
such as steroids. This form of Glaucoma may be mild or severe. The type of treatment will depend on
whether it is Open Angle Glaucoma or Angle Closure
Glaucoma.
Normal Tension Glaucoma (NTG)
Normal Tension Glaucoma is also known as Low
Tension Glaucoma, or Normal Pressure Glaucoma. In
this type of Glaucoma, the Optic Nerve is damaged,
even though intraocular pressure (IOP) is not very
high. Those at higher risk for this form of Glaucoma
are people with a family history of Normal Tension
Glaucoma, people of Japanese ancestry, and people
with a history of Systemic Heart Disease, such as
irregular heart rhythm. Normal Tension Glaucoma is
usually detected after an examination of the optic
nerve.
Pigmentary Glaucoma
This is a form of secondary Open Angle Glaucoma. It
occurs when the pigment granules in the back of the
Iris (the colored part of the eye) break into the clear
fluid produced inside the eye. The tiny pigment
granules flow toward the drainage canals in the eye
and slowly clog them, causing the eye pressure to rise.
Treatment usually includes medication or surgery.
HEMIANOPIA
Blindness affecting half of the field of vision.
Hemianopia, also known as hemianopsia, may be
caused by various medical conditions, but usually
results from a stroke or brain injury. It may affect either the right or left side of the visual field and is
usually permanent. Hemianopia can produce various
effects, from minor to severe. For example, a person
may be able to see only to one side when looking
ahead, or objects that the person sees may differ in
clarity or brightness. Such visual impairment can make
it difficult to perform daily tasks, from reading to
crossing streets. There is no specific treatment for
hemianopia, but low vision rehabilitation specialists
can help people learn to make the most of the sight
that they have. In addition, some people with
hemianopia benefit from the use of magnifiers or
special prism lenses.
HISTOPLASMOSIS
Histoplasmosis is a disease caused when airborne
spores of the fungus Histoplasma capsulatum are
inhaled into the lungs, the primary infection site. This
microscopic fungus, which is found throughout the
world in river valleys and soil where bird or bat
droppings accumulate, is released into the air when soil
is disturbed by plowing fields, sweeping chicken coops,
or digging holes. Histoplasmosis is often so mild that it
produces no apparent symptoms. Any symptoms that
might occur are often similar to those from a common
cold. In fact, if you had histoplasmosis symptoms, you
might dismiss them as those from a cold or flu, since
the body’s immune system normally overcomes the
infection in a few days without treatment. However, histoplasmosis, even mild cases, can later cause a
serious eye disease called ocular histoplasmosis
syndrome (OHS), a leading cause of vision loss in
Americans ages 20-40.
OHS develops when fragile, abnormal blood vessels
grow underneath the retina. These abnormal blood
vessels form a lesion known as choroidal
neovascularization (CNV). If left untreated, the CNV
lesion can turn into scar tissue and replace the normal
retinal tissue in the macula. The macula is the central
part of the retina that provides the sharp, central vision
that allows us to read a newspaper or drive a car.
When this scar tissue forms, visual messages from the
retina to the brain are affected, and vision loss results.
Although only a tiny fraction of the people infected with
the histo fungus ever develops OHS, any person who
has had histoplasmosis should be alert for any changes
in vision. Studies have shown the OHS patients usually
test positive for previous exposure to histoplasmosis.
In the United States, the highest incidence of
histoplasmosis occurs in a region often referred to as
the “Histo Belt,” where up to 90 percent of the adult
population has been infected by histoplasmosis. This
region includes all of Arkansas, Kentucky, Missouri,
Tennessee, and West Virginia as well as large portions
of Alabama, Illinois, Indiana, Iowa, Kansas, Louisiana,
Maryland, Mississippi, Nebraska, Ohio, Oklahoma,
Texas, and Virginia. Since most cases of histoplasmosis
are undiagnosed, anyone who has ever lived in an area
known to have a high rate of histoplasmosis should consider having their eyes examined for histo spots.
More info on this topic may be found at the National
Eye Institute: www.nei.nih.gov/
Ocular histoplasmosis requires no treatment except
when abnormal blood vessels develop in the central
retina. For these patients, laser treatment, intraocular
injections, or vitrectomy surgery may be necessary.
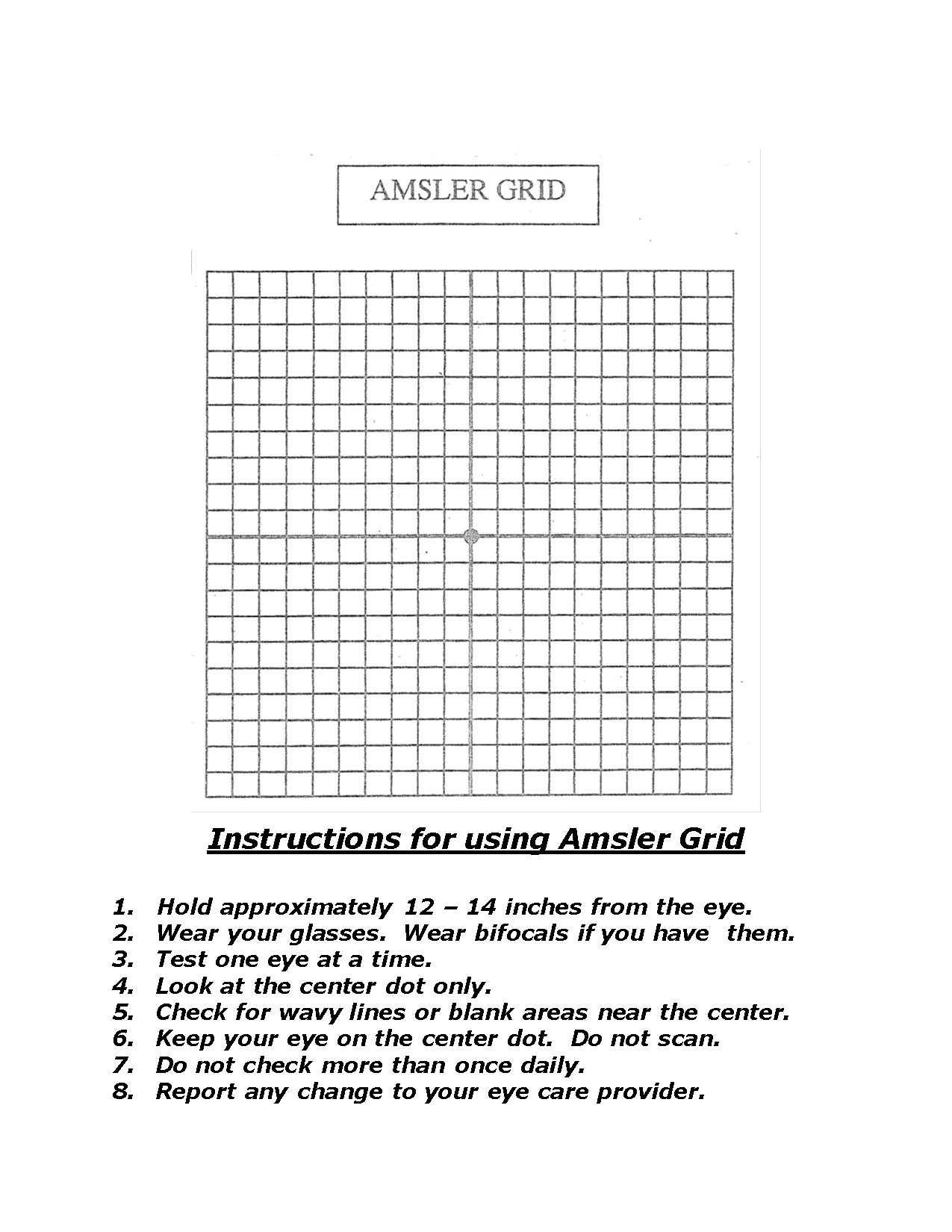
Regular eye exams and routine use of an Amsler Grid to
monitor central vision is recommended for anyone with
histo spots. For your convenience, there is an Amsler
Grid at the end of this chapter.
MACULAR DEGENERATION
Age-Related Macular Degeneration
Age-related Macular Degeneration (AMD) is a disease
that blurs the sharp, central vision you need for
“straight ahead” activities such as reading, sewing, and
driving. AMD affects the macular, the part of the eye
that allows you to see fine details. In some cases, AMD
advances so slowly that people notice little changes in
their vision. In others, the disease progresses faster
and may lead to loss of vision in both eyes. AMD is a
leading cause of vision loss in Americans 60 years of
age and older.
Wet AMD
Wet AMD occurs when abnormal blood vessels behind
the retina start to grow under the macula. These new
blood vessels tend to be very fragile and often leak
blood and fluid. The blood and fluid raise the macula from its normal place at the back of the eye. Damage
to the macula occurs rapidly. With Wet AMD, loss of
the central vision can occur quickly. Wet AMD is
considered to be advanced AMD and is more severe
than the dry form. An early symptom of Wet AMD is
that straight lines appear wavy.
Dry AMD
Dry AMD occurs when the light-sensitive cells in the
macula slowly break down, gradually blurring central
vision in the affected eye.
As Dry AMD gets worse, you may see a blurred spot
in the center of your vision. Over time, as less of the
macula functions, central vision in the affected eye can
be lost gradually. The most common symptom of Dry
AMD is slightly blurred vision. You may have difficulty
recognizing faces. You may need more light for
reading and other tasks. Dry AMD generally affects
both eyes, but vision can be lost in one eye while the
other seems unaffected. Dry AMD has three stages, all
of which occur in one or both eyes.
Early AMD
People with Early AMD have either several small drusen or a few medium-sized drusen. At this stage, there are
no symptoms and no vision loss.
Intermediate AMD
People with Intermediate AMD have either many medium-sized drusen or one or more large drusen.
Some people see a blurred spot in the center of their vision. More light may be needed for reading.
Advanced Dry AMD
In addition to druse, people with Advanced Dry AMD have a breakdown of light- sensitive cells and supporting tissue in the central retinal area. This breakdown can cause a blurred spot in your vision. Over time, the blurred spot may get bigger and darker, taking more of your central vision. You may have difficulty reading or recognizing faces until they are very close to you. *If you have vision loss from Dry AMD in one eye only, you may not notice any changes in your overall vision, only if AMD affects both eyes.
RETINITIS PIGMENTOSA
Retinitis Pigmentosa is an eye disease that affects a person’s night vision and peripheral vision. It is a
genetic disorder that is usually hereditary. Symptoms start with decreased night vision and later progresses to a diminishing of peripheral vision. The rate of decline varies depending on the genetic makeup of the disorder, and also varies somewhat in individuals. You will find the Amsler Grid at the end of this chapter – page 26. If you have been diagnosed with Retinitis Pigmentosa, and whether you have noticeable impaired Peripheral Vision, you should periodically use this Amsler Grid to note changes in your eyesight. Make note of any wavy lines or missing areas. While keeping your eye on the center dot, can you see all four corners of the Amsler Grid?
STARGARDT DISEASE
Stargardt Disease is the most common form of inherited Juvenile Macular Degeneration. It is characterized by the reduction of Central Vision with a preservation of Peripheral (side) Vision. Stargardt Disease is usually diagnosed in individuals under the age of 20 when decreased central vision is first noticed. On examination, the retina of an affected individual shows a macular lesion surrounded by yellow-white flecks, or spots, with irregular shapes. Eventually, almost all with Stargardt disease are expected to have visual acuities in the range of 20/200 to 20/400. The reduced visual acuity due to Stargardt Disease can’t be corrected with prescription eyeglasses or contact lenses. In late stages of the disease, there may also be noticeable impairment of color vision. Stargardt Disease is almost always inherited as an Autosomal Recessive Disorder. It is inherited when both parents, called carriers, have one gene for the disease paired with one normal gene. Each of their children has a 25% chance of inheriting the two copies of the Stargardt gene (one from each parent) which is needed to cause the disease. Carriers are unaffected because they have only one copy of the gene.
Although there is currently no treatment of Stargardt Disease, individuals may benefit from the use of low vision aids, plus orientation and mobility training.
*Please check the Amsler Grid at the end of this chapter.
USHER SYNDROME
Usher syndrome is the most common condition that affects both hearing and vision. A syndrome is a disease or disorder that has more than one feature or symptom. The major symptoms of Usher syndrome are hearing loss and an eye disorder called retinitis pigmentosa, or RP. RP causes night-blindness and a loss of peripheral vision (side vision) through the progressive degeneration of the retina. The retina is a light-sensitive tissue at the back of the eye and is crucial for vision. As RP progresses, the field of vision narrows—a condition known as “tunnel vision”—until only central vision (the ability to see straight ahead) remains. Many people with Usher syndrome also have severe balance problems.
By registering in the USH Trust, you will become part of the largest global network of individuals with Usher syndrome. You will have the opportunity to contribute to the world's understanding of Usher syndrome, will be ensured of receiving information on the latest research, treatments and clinical trials, and will be the first to learn about opportunities to participate in research.
https://www.usher-registry.org